Hernández-García M, Nieto-Torres M, Guerra-Pinto N, Castillo-Polo JA, Saez de la Fuente J, Michelena M, Ponce-Alonso M, Soriano-Cuesta C, Díaz-Agero C, Cantón R, Coque TM, Ruiz-Garbajosa P. ICU environment as a reservoir of KPC-ST307-Klebsiella pneumoniae high-risk clone resistant to ceftazidime-avibactam
Sci Rep. 2025
"ICU environment was a hidden driver in the transmission and evolution of last-line antibiotic resistance in KPC-K. pneumoniae during the COVID-19 pandemic". - Dr. Marta Hernández García
Summary:
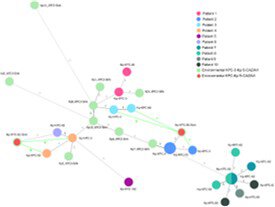
We characterized all ceftazidime-avibactam-resistant KPC-producing K. pneumoniae (KPC-Kp) isolates recovered from both patients and environmental samples at the ICU of our hospital in 2020, during the COVID-19 pandemic initiation. Antimicrobial susceptibility testing and whole genome sequencing analysis were performed. Ten patients (16% of ICU patients) were colonized or infected by a ceftazidime-avibactam-resistant KPC-Kp isolate from March to December 2020, six of them during or after treatment with ceftazidime-avibactam. Two ceftazidime-avibactam-resistant KPC-Kp were also recovered from two ICU sinks between July and September. All isolates belonged to ST307 clone and had identical resistance gene content. Six different KPC variants (KPC-62, KPC-92, KPC-150, KPC-66, KPC-53, KPC-46) were detected in patient isolates. KPC-92 and KPC-66 variants were also found in sink isolates. Regardless of the origin (patients or sinks), KPC-92-Kp, KPC-150-Kp and KPC-62-Kp isolates combining altered porin proteins also exhibited increased or resistant MIC values to novel antimicrobials, such as cefiderocol, cefepime-taniborbactam, aztreonam-avibactam, meropenem-vaborbactam and/or imipenem-relebactam. A cgMLST analysis demonstrated the clonal spread of KPC-ST307-Kp within the ICU, between patients and the hospital environment. Clustering was observed mainly by KPC variants (KPC-92, KPC-62). A variant calling analysis and plasmid characterization showed possible transmission between patients and sinks. Our results suggest that the patient care environment likely contributed to persistence and spread of last-line antibiotics-resistant KPC-Kp within the ICU during the COVID-19 pandemic.
Why do you highlight this publication?
Our study reveals the ICU environment served as a critical reservoir for the high-risk clone KPC-ST307 K. pneumoniae during the COVID-19 pandemic, with the emergence of resistance to last-line antibiotics posing major therapeutic challenges. We documented evidence of potential transmission events between patients and ICU sinks, underscoring the environment's role in the persistence and dissemination of multidrug-resistant organisms-an issue recently emphasized by the United Nations Environment Programme. Our findings contribute to the understanding of the evolution of resistance to novel β-lactam/β-lactamase inhibitor combinations in KPC-K. pneumoniae isolates and their impact on patient care, while highlighting the need to strengthen infection control measures, disinfection strategies, and environmental surveillance in critical care units to mitigate the global health threat posed by these pathogens.
Publication commented by:
Dr. Marta Hernández García
BIOLOGY AND EVOLUTION OF MICROORGANISMS. IRYCIS
CIBERINFEC (CB21/13/00084)