Bayona A, Nattero L, De la Calle E, Quintero A, de Lope S, Dorado B, Fiers T, Kaufman JM, Luque M, Escobar HF. Androgen excess disorders remain undiagnosed in one of every four premenopausal women with Type 1 diabetes
Hum Reprod Open. 2025
"Androgen excess disorders are the most commonly ignored associations of type 1 diabetes in women by far" Ane Bayona & Dr. Héctor Escobar
Summary:
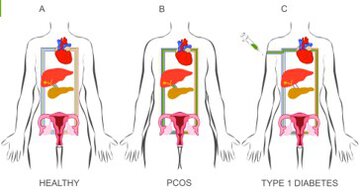
Study question: How frequent are androgen excess disorders, including polycystic ovary syndrome (PCOS), among women with Type 1 diabetes mellitus (T1D)?
Summary answer: One in every four women with T1D suffer from undiagnosed androgen disorders, with the classic phenotype of PCOS being the most frequent.
What is known already: Systemic iatrogenic hyperinsulinism is unavoidable in patients with T1D because insulin is administered subcutaneously instead of being secreted directly into the portal circulation. Since insulin acts as a co-gonadotrophin at the ovary, iatrogenic hyperinsulinism might trigger androgen secretion in predisposed women. Most studies conducted to date have reported increased prevalences of androgen excess disorders in premenopausal women with T1D, yet these studies were hampered by methodological limitations that preclude reaching a definite conclusion on the issue.
Study design size and duration: From January 2020 to March 2024, we conducted a cross-sectional study including women with T1D.
Participants setting methods: We recruited 149 consecutive premenopausal women with T1D who attended the diabetes clinics of an Academic Hospital at Madrid, Spain. We compared them with 295 typical patients with PCOS who did not have T1D. We used state-of-the-art mass spectrometry techniques to measure serum androgens and equilibrium dialysis to measure free testosterone and followed the latest guidelines to phenotype patients.
Main results and the role of chance: Hyperandrogenic disorders (considering PCOS, idiopathic hyperandrogenism, and idiopathic hirsutism as a whole) were present in 39 (of 149) women with T1D (26%, 95% CI: 20-34%), including 30 women who fulfilled the PCOS diagnostic criteria, indicating a prevalence of 20% (95% CI: 15-27%). The most common PCOS phenotype was the classic combination of hyperandrogenism and ovulatory dysfunction. Women with T1D and PCOS were younger (mean age 25 ± 7 vs 31 ± 9 years-old, P = 0.003) and their onset of T1D was more frequently premenarcheal (73% vs 46%, P = 0.008) compared to those without PCOS. Compared to 295 typical patients with PCOS without T1D, the 30 women with T1D and PCOS showed milder hyperandrogenic signs and lower free testosterone concentrations [13 (9, 25) vs 21 (15, 29) pM, P < 0.001] regardless of the glucose tolerance of the former.
Wider implications of the findings: One in every four women with T1D suffer androgen excess disorders, with the classic combination of hyperandrogenism and ovulatory dysfunction being the most common phenotype of PCOS. Women with a premenarcheal onset of T1D are particularly susceptible to developing androgen excess disorders and may benefit from future preventive measures at young ages. Routine screening for these prevalent disorders seems reasonable to avoid the negative consequences of androgen excess and chronic ovulatory dysfunction on the general and reproductive health of T1D women.
Why do you highlight this publication?
We firstly described the association of type 1 diabetes and androgen excess disorders such as PCOS in year 2000. Since our initial description, this association has been routinely confirmed by all but one of the many studies conducted to date. Our present study not only confirmed that one in every four women with type 1 diabetes suffers from an undiagnosed androgen excess disorder - with the most severe classic PCOS phenotype reaching an striking 20% prevalence - but also addressed all possible caveats of earlier studies by applying state-of-the-art methodology for the assessment of androgen concentrations and polycystic ovarian morphology. Discouragingly, screening for these very prevalent androgen excess disorder is not recommended nowadays by any clinical guideline for the management of type 1 diabetes. We hope that this article, together with earlier meta-analyses by our group, would promote the visibility of the problem, its early detection, and the avoidance of the negative consequences of androgen excess and chornic ovulatory dysfunction on the general and reprodyctive health of women with type 1 diabetes.
Publication commented by:
Ane Bayona Cebada & Dr. Héctor Escobar Morreale
DIABETES, OBESITY AND HUMAN REPRODUCTION group. IRYCIS