Vizcarra P, Pérez-Elías MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, Casado JL; COVID-19 ID Team. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort.
The Lancet HIV. 2020
"HIV-infected individuals should not be considered to be protected from SARS-CoV-2 infection or to have lower risk of severe disease, as previously proposed". - Dra. Pilar Vizcarra -
Summary:
BACKGROUND: Information about incidence, clinical characteristics, and outcomes of HIV-infected individuals with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is scarce. We characterised individuals with COVID-19 among a cohort of HIV-infected adults in Madrid.
METHODS: In this observational prospective study, we included all consecutive HIV-infected individuals (aged ≥18 years) who had suspected or confirmed COVID-19 as of April 30, 2020, at the Hospital Universitario Ramón y Cajal (Madrid, Spain). We compared the characteristics of HIV-infected individuals with COVID-19 with a sample of HIV-infected individuals assessed before the COVID-19 pandemic, and described the outcomes of individuals with COVID-19.
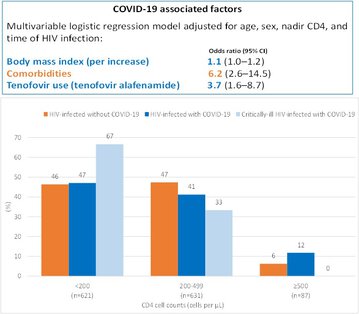
FINDINGS: 51 HIV-infected individuals were diagnosed with COVID-19 (incidence 1·8%, 95% CI 1·3-2·3). Mean age of patients was 53·3 years (SD 9·5); eight (16%) were women, and 43 (84%) men. 35 (69%) cases of co-infection had laboratory confirmed COVID-19, and 28 (55%) required hospital admission. Age and CD4 cell counts in 51 patients diagnosed with COVID-19 were similar to those in 1288 HIV-infected individuals without; however, 32 (63%) with COVID-19 had at least one comorbidity (mostly hypertension and diabetes) compared with 495 (38%) without COVID-19 (p=0·00059). 37 (73%) patients had received tenofovir before COVID-19 diagnosis compared with 487 (38%) of those without COVID-19 (p=0·0036); 11 (22%) in the COVID-19 group had previous protease inhibitor use (mostly darunavir) compared with 175 (14%; p=0·578). Clinical, analytical, and radiological presentation of COVID-19 in HIV-infected individuals was similar to that described in the general population. Six (12%) individuals were critically ill, two of whom had CD4 counts of less than 200 cells per μL, and two (4%) died. SARS-CoV-2 RT-PCR remained positive after a median of 40 days from symptoms onset in six (32%) individuals, four of whom had severe disease or low nadir CD4 cell counts.
INTERPRETATION: HIV-infected individuals should not be considered to be protected from SARS-CoV-2 infection or to have lower risk of severe disease. Generally, they should receive the same treatment approach applied to the general population.
Why do you highligth this publication?
This was the first study to comprehensively describe the infection rate of COVID-19 in people living with HIV compared with the general population in the same region. Additionally, it underscored the high prevalence of comorbidities among HIV-infected individuals with COVID-19. Lower CD4 cell counts affected disease severity and viral kinetics. Age-adjusted mortality was higher in our cohort than that described in the general population in the same region.
Publication commented by:
Dra. Pilar Vizcarra
Department of Infectious Diseases,
Hospital Universitario Ramón y Cajal